If you are an Inflammatory Bowel Disease (IBD) patient, and you’ve experienced hair loss, you are not alone
A recent cross-sectional study found that “Thirty-three percent of [IBD] patients reported a history of hair loss”. 1http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/
Count me in as one of those 33%!
But, what causes an IBD patient to lose hair?
There are multiple factors to consider when an IBD patient is experiencing hair loss. Many patients have reported hair loss as a side effect of medications used to treat their IBD.2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/ And, some medications can be associated with hair loss in some patients. 3http://www.ncbi.nlm.nih.gov/pubmed/19420815/ But hair loss in Inflammatory Bowel Disease is also associated with nutritional deficiencies, hormonal imbalances, and both acute and chronic illness.4http://www.ncbi.nlm.nih.gov/pubmed/23624889
The focus of this article will not be to look at all possible factors that contribute to hair loss in IBD. Just like IBD, itself, hair loss associated with IBD is a complex thing that needs to be addressed on a patient-to-patient basis with the help of qualified medical professionals. However, I would like to focus on the one thing that is associated with most cases of hair loss in IBD patients: the IBD, itself.
Hair loss can be a symptom of Inflammatory Bowel Disease
Hair loss has been observed in IBD patients enough over the years, that it can be considered an extra-intestinal (meaning outside of the intestines) symptom of Crohn’s disease and ulcerative colitis 5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/. Although not a terribly common scenario, hair loss can actually be the first recognizable symptom of Inflammatory Bowel Disease for some patients.6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292143/ 7http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/
Although hair loss has long been reported by IBD patients and observed in various studies, it’s still a lesser known and understood aspect of Crohn’s and ulcerative colitis. Fortunately, thanks to ongoing research and an ever-improving understanding of these diseases, there are some basic things we can understand about hair loss in IBD.
In 2013, Guy’s and St Thomas’ Hospital in London conducted a scientific literature search spanning 46 years (1966-2012) to better understand the prevalence of hair loss experienced by IBD patients. Their search found that:
“Telogen effluvium associated with acute or chronic flares of IBD is probably the commonest cause of disease-related hair loss…” 8http://www.ncbi.nlm.nih.gov/pubmed/23624889
So, this thing called “Telogen Effluvium”, which is associated with active disease in Crohn’s and ulcerative colitis, looks to be the most common cause of hair loss among IBD patients…
——————
Ok, so what is Telogen Effluvium?
To understand Telogen Effluvium, we have to know a little about the growth phases of hair. When describing the growth of human hair, there are three basic phases: anagen, catagen, and telogen. 9http://emedicine.medscape.com/article/1073488-overview Anagen is the “growth” phase of hair, catagen is the “transitional” phase, and telogen is the “resting” phase of hair. Individual hairs start in the anagen (growth) phase, then become catagen (transitional), and finally become telogen (resting) before being shed to make room for new anagen (growth) hair. Catagen is a very brief phase 10http://emedicine.medscape.com/article/1073488-overview and, for the sake of this article, we only need to worry about the anagen (growth) and telogen (resting) phases.

Resting hair
To put it simply:
- The anagen, “growth”, phase is when your hair is actively growing (complicated stuff, I know 😉 ).
- The telogen, “resting”, phase is when your hair is not growing (shhhh… it’s resting! 😆 )
When you’re healthy, the vast majority of hair on your head will be in the anagen phase at any given time, while about 5-15% of your hair will be in the telogen phase. 11http://emedicine.medscape.com/article/1071566-overview#a0104
There can be quite a bit of variation in how long these phases last in people, but typically the anagen (growth) phase lasts about three years, while the telogen (resting) phase lasts about three months. 12http://emedicine.medscape.com/article/1071566-overview#a0104
Look at all of that telogen hair!
When a hair is in the telogen (resting) phase, it remains where it’s at for a few months or so, until it’s shed to make room for new anagen (growth) hair. 13http://emedicine.medscape.com/article/1071566-overview#a0104 So, if you normally only have 5-15% of your hairs in telogen (resting) phase at any given time, you probably won’t be noticing much difference in the thickness of your hair even as you are actively shedding it to make room for new anagen growth.
But what if a lot more than 5-15% of your hair is in telogen (resting) phase?
Well, then you’re definitely going to notice when all of that telogen hair falls out to make way for new anagen hair! And, that is when “Effluvium” comes in to play. Effluvium means “an outflowing or shedding, as of the hair”. 14http://medical-dictionary.thefreedictionary.com/effluvium So, “Telogen Effluvium” refers to a noticeable outflowing or shedding of telogen hair.
But, what triggers this mass shedding of telogen hair?
According to Dermatologist Elizabeth CW Hughes, MD:
“Telogen effluvium is triggered when a physiologic stress or hormonal change causes a large number of hairs to enter telogen at one time. Shedding does not occur until the new anagen hairs begin to grow. The emerging hairs help to force the resting hairs out of the follicle. […] The interval between the inciting event in telogen effluvium and the onset of shedding corresponds to the length of the telogen phase, between 1 and 6 months (average 3 mo).” 15http://emedicine.medscape.com/article/1071566-overview#a0104
Ok, let’s break this down a bit:

Don’t make any sudden movements.
You know how when you’re in a stressful or frightening situation, you can go into “fight or flight” mode, which causes your body to stop focusing on mundane, everyday tasks like digestion and, instead, prepare the body to run from or fight off a lion? 16http://www.ncbi.nlm.nih.gov/pubmed/7570024 That’s an acute stress response. (And that’s a cute lion →)
Well, Telogen Effluvium could be looked at as an extreme sort of stress response 17http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1868104/ 18http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2111110/
This is an oversimplification, but in many cases of Telogen Effluvium, it’s like your body is under so much “stress” that it decides it can’t focus on growing hair right now. For IBD patients, that “stress” is likely active disease and/or surgery. 19http://www.ncbi.nlm.nih.gov/pubmed/23624889 20http://journals.lww.com/anesthesia-analgesia/Citation/1984/01000/Telogen_Effluvium_after_Anesthesia_and_Surgery_.17.aspx
Of course, Telogen Effluvium can also be associated with hormonal changes. But, Inflammatory Bowel Disease is also strongly associated with hormonal changes and problems 21http://www.ncbi.nlm.nih.gov/pubmed/6384458 22http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3959350/. So, in many ways, we keep coming back to the IBD, itself.
To summarize, here is roughly what happens when you lose hair due to Telogen Effluvium:
- Physiologic stress or hormonal change occurs (possibly because of active or recently active Crohn’s or ulcerative colitis, or surgery)
- This triggers a large number of hairs to enter telogen (resting) phase
- The telogen (resting) hair begins shedding around the end of a typical telogen phase (1-6 months)
Pay close attention to #3 above. With Telogen Effluvium, you are shedding your telogen hair pretty much like you always do: 1-6 months after it enters the telogen phase. The difference is that far more of your hair is in a telogen state. This means that you will lose a lot of hair in a relatively short amount of time. It also means that you may mistake the cause of your hair loss, because it was triggered by something that happened months earlier!
This is the really important part to understand, so I’m going to say it again in much bigger letters in a fancy quote box, and then I’m going to reiterate it with some nice images:
You may mistake the cause of your hair loss, because it was triggered by something that happened months earlier!

You might think your hair loss is caused by these

When it’s actually the result of active Crohn’s disease or ulcerative colitis, or surgery
Here is a possible scenario that may happen because of this:
- An IBD patient enters a severe flare-up of his disease, which triggers a large amount of his hair to enter the telogen phase.
- One month later, the patient is started on a new medication to treat his severe IBD.
- Another month passes. The new medication is starting to help control the damaging inflammation caused by his IBD. Coincidentally, all of his hair that was in telogen phase is shed to make room for new anagen growth (as it generally does after 1-6 months), causing massive hair loss.
- The patient assumes the new medication is causing the hair loss, when in fact, the severe IBD, which is now being managed by said medication, is what triggered the hair loss.
- The patient becomes non-compliant (stops taking the new medication), or insists to his doctor that he needs to be taken off his medication because of the hair loss.
This is just one possible scenario, but it does happen. I have made the mistake, in the past, of thinking my hair loss was caused by a new medication. Fortunately, I had a knowledgeable doctor who was able to confidently explain Telogen Effluvium to me. He provided me with reassurance (something we will come back to) that my hair loss was not permanent. And he also reminded me how important it is to control any damage being caused by my Crohn’s disease.
The purpose of this article is not to convince people that medications can’t cause hair loss.
There have been associations found between certain medications and hair loss. 23http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0014051/ 24http://www.ncbi.nlm.nih.gov/pubmed/11305380 But, associations do not mean that one thing caused the other. With more research being done, it is becoming clear that medications are not to blame as much as we might have once suspected. 25http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/
IBD medications like Remicade (infliximab) and mesalamines may help prevent hair loss in patients
A very recent cross-sectional study showed that IBD patients who had been on anti-TNF medications (for example, but also most significantly, Remicade) and/or mesalamines (aka 5-ASA drugs, like Lialda) were actually less likely to have experienced hair loss. 26http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/ In addition, they did not find a difference in hair loss between patients that had been on immunomodulators, or steroids, and those that hadn’t. 27http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/#__sec5title.
And, very notably, among the patients included in the study:
“Sixty-two percent of patients with hair loss experienced their hair loss around the time of an IBD flare.”28http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284339/#__sec5title
So, here we see more evidence to suggest that hair loss in Inflammatory Bowel Disease tends to be associated with the state of the disease itself. But, hair loss is very distressing, whether or not you know what triggered it! I’ve experienced significant hair loss on multiple occasions over the years, even as a child, so I know this from first-hand experience. If you’re like me, knowing what Telogen Effluvium is will not be enough. You will want to know:
Will my hair grow back if I have Telogen Effluvium?
While losing hair is absolutely an unwanted additional stressor on top of already being sick, it’s important to receive reassurance that, in most cases, your hair will grow back in time. According to Dr. Hughes:
“Because acute telogen effluvium is a reactive process, which resolves spontaneously, treatment usually is limited to reassurance.” 29http://emedicine.medscape.com/article/1071566-treatment
In other words, as long as the underlying cause is treated (which, in the case of IBD patients, is most commonly associated with active disease), the telogen effluvium will resolve itself.
Now, let’s tie all of this knowledge together by looking at a real-world example
Hearing about a documented case of hair loss and regrowth in another IBD patient may help provide you with some reassurance. Well, here is just such an example of a recent case study about a child with Crohn’s disease:
“Telogen effluvium was the first symptom of Crohn’s disease in a child, and […] should be considered as an extraintestinal manifestation of Crohn’s disease.” 30http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/
This 10 year old girl experienced Telogen Effluvium one year prior to her diagnosis with Crohn’s disease. Being that it is an extra-intestinal manifestation of Crohn’s disease, it was one of the signs that led to her finally being diagnosed.
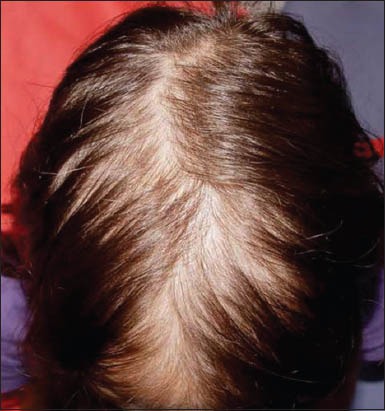
10 year old girl with Telogen Effluvium caused by active Crohn’s disease 31http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/
Here is what her hair looked like before she began treatment for her Crohn’s disease:

10 year old girl, one year after receiving proper medical care for her Crohn’s disease (which was the cause of hair loss) 32http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/
And here is what her hair looked liked one year later, after receiving proper medical treatment (involving Remicade, immunomodulators, and steroids) for her Crohn’s disease (the underlying cause of the Telogen Effluvium):
Here are some main points to take away from this article:
- Hair loss is a common problem among IBD patients.
- Telogen Effluvium associated with active IBD seems to be the most common cause of hair loss among patients.
- Telogen Effluvium can seem like it’s caused by something other than active disease or surgery (such as medications) because of the timing of hair loss.
- Telogen Effluvium hair loss is reversible.
- If you experience hair loss, discuss it with your doctor. Please do not make any decisions about your IBD treatment without discussing it with the physician treating it. This part is important, so it bears repeating in bigger letters:
If you have IBD and you’ve begun experiencing hair loss, please speak with your doctor about it.

Speak to your doctor about hair loss
There are many reasons why an IBD patient may be losing hair, and it’s important to work with a qualified medical team to determine the cause so you can work towards a solution. Fortunately, the causes of hair loss generally associated with IBD, such as nutritional deficiencies, hormonal imbalances 33http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4188947/, side effects of medications, and acute and chronic illness, can be reversed. 34http://emedicine.medscape.com/article/1071566-treatment
References



Great article! Very thorough. Interesting that hair loss can be a symptom of crohns, not necessarily from medication as I had always thought.
This was great. I’ve experienced hair loss twice and this article makes so much sense. Thanks for posting.
Thanks for reading! I’m glad you got something out of it!
This had been happening to me over the last couple months. My doctor prescribed me a specific vitamin b supplement a couple weeks ago and that has really helped. Definitely talk to your doctor before taking anything, but they might be able with some of the hair loss.
Which vitamin b was it so that I may try it thank you.
Nice job sharing this research Dan. When my hair fell out back in 1987 nobody had ever seen this, or so it seemed. What was odd then was the hair would fall out, grow back in and fall out again. When it grew back it felt very different, so it didn’t surprise me when it fell out again. But after having surgery and getting my health back, the hair was never again an issue. Can’t say the same for my intestines, but the hair stayed put at least.
Happy to share, Matthew. It’s amazing how much more is known about IBD and its many effects on the body now as compared to, say, 1987. I’m glad to hear your hair has stayed put since surgery! Stories like that can help bring reassurance to other patients experiencing Telogen Effluvium.
can this process last longer than 6 months, i havnt had ibd just stress
Hi Antonio, I’m sorry to hear you’ve been experiencing hair loss. Yes, the hair loss process involved in Telogen Effluvium can last longer than six months. There are various ways that Telogen Effluvium can occur, and some are more chronic in nature. In any case, it’s important to address the underlying causes/triggers. If you haven’t already, please ask your doctor about your hair loss. Best of luck to you!
Pingback: IBD Fact #23: Hair loss can be a symptom of IBD • Dan Sharp
OMG! Huge thanks for posting this! Was just at dr talking about this today! I was trying to get him to lower my Remicade, when he mentioned several recent studies regarding hair loss and IBD.
You’re very welcome, Lisa! Thanks for commenting.
Debido a efecto secundario de humira para enfermedad de crohn he tenido brote de soriasis, en mi cuero cabelludo han salido muchas costras y el pelo cae junto con ellas. Tengo zonas rojas y sin pelo!!! Los mechones de pelo están enganchados a la costra. Volverá a salirme el pelo en estás zonas?
I’ve noticed that I lost hair over the last few months. I’m a 30 year old male with UC, and no history of genetic baldness among my parents, grandparents, nor great-grandparents.
We shall see. I’m hoping the hair will come back. Thanks for posting this thoughtful article with citations.
Hey Richard, thanks for the comment. I’m sorry to hear about your hair loss. I know the waiting and hoping can be quite distressing, so I hope things are back to normal for you soon. Have you talked to your GI about it?
Thank you so much for this article makes so much sense. \i did talk to my GI today and he also explained it was more than likely caused from when i was having a flare not the new meds. Thanks again for taking the time to post this
Thank you for the nice feedback, Kathy. I’m glad your GI explained what was going on!
I’ve had 4 lots of surgery for my Crohn’s disease and have been really unwell in the past. I never lost any hair at all during these times, even when my weight dropped to well under six stone. Then my Consultant decided put me on infliximab infusions every eight weeks and that is when my hair loss started. I now have very thin and brittle hair which is devastating when it was once beautifully strong with lots of it. So depressing. When I’ve mentioned this ( on more than one occasion ) to GP’s at my medical practice, their eyes just glaze over.
Thanks for the awesome article. I’m experiencing hairloss at the moment and I am unsure if its genetic or due to the IBD. I have had many flares throughout the year so after reading this I’m thinking my hairloss could be due to me not being well. I’ve been feeling better after started Remicade 3 days ago. Does the pattern of hairloss determine if it’s due to the IBD or maybe genetics? I have had most of the hairloss on my scalp and only a really small amount on the sides. I also have a receding hairline but only on my right side. Hopefully since my health is better it helps my hair, thanks for helping us understand how hairloss ca affect us with IBD.
Love your post,you did a great job explaining this for this unfortunate condition. in your opinion, does the hair loss stem from the flare up it self or the poor nutritional status of the person during the flare? My 29 year old daughter started to flare in December. Lost 20 pounds in 7 months. The colonoscopy revealed on a small inflamed section (less than 2 inches). Still not in remission, but able to tolerate food now. Which is more likely the causing factor?
Thank you in advance for your help
I just found your website while trying to understand my 15 year old’s hair loss from UC. Thank you for all your work on behalf of individuals and families living with IBD. I am a nursing professor and plan to share your site with my students so they can see how individuals living with a chronic condition can learn how to create a healthcare team that works with them to achieve their health goals. Very inspiring story!
Question- so fkare ups and poor nutritional status can lead to hair loss, what can be done to help prevent this in the future and promote hair growth ty
Hi Patricia. This would be an important topic to discuss with one’s physician. However, I think it’s safe to say that properly treating one’s IBD (ideally, with a GI who specializes in IBD) and maintaining good nutritional status (a Registered Dietitian with experience in IBD could help a lot) are important steps to take in order to achieve and maintain relatively good health (which will help prevent future hair loss episodes).
Thanks for your nice feedback, Anne-Marie! I really appreciate you sharing my site with your students. I’m sorry to hear your child has lost hair from UC; I hope things are looking up now.
This is fascinating and something I have never read up on much. Thanks Dan.
Hi Dan..thanks for the article. I have also been experiencing hair loss with UC over the past 4/5 years, however, mine doesn’t appear to be growing back? …can this happen tomorrow? Some days I feel heartbroken, other days I kick myself for being selfish and vein…..I just didn’t expect to lose so much hair by 36! Emma x
I mean too*…not tomorrow..sorry!
Hi Emma, I’m very sorry you’re dealing with unresolved hair loss! If you haven’t already, please make sure you’re letting your physician know what’s going on and how detrimental it is to you. Hair loss can be very distressing, and you’re not selfish or vain for being upset over it. If your UC is not being well controlled, that would certainly be something to address in any case; but only your medical team can determine what the exact cause of the hair loss is.
If you feel your GI is not taking your hair loss issue seriously, or is unsure of what to do, you may want to consider speaking with another physician. Your primary care provider/GP, or someone they refer (such as a Dermatologist) are options to consider. Good luck!
Thank you. I was med non compliant for a while because i thought it was messing with my nutrient intake and thus making my hair fall out. My doctor asked me to reframe that in my head because the meds were upping the nutrition I was absorbing and easing flares. Since I have been very strict about taking my meds, my hair is looking fuller.
That’s great to hear! Thanks for sharing!
I found this research article in an online support group. It explained a lot, and eased my mind (as much as it can be) about my hair loss. I have always had super thick hair. I have Crohn’s Disease and this summer I had an Obscure GI Bleed which landed me in the hospital for 37 days, 27 RBC transfusions, 3 FFP transfusions, and 2 platelet transfusions, and four surgeries. I had massive amounts of medications and very little nutrition until the TPN finally came along. I am still having absorption issues. Massive amount of hair has been lost, and I now have pretty thin hair. I am working with my GI, as I flared after I got out of the hospital. We need to get the nutrition back in check. The past day or two there hasn’t been noticeable loss, so hopefully I’m on the way back up. My body has been through hell and back since May. The hair loss started the beginning of August ( a month and a half after getting out of the hospital) — this makes sense based on the research in this article.
Sorry this is so long. I am relieved by this article, and apparently I need to be patient for it to grow back. Thank you!
Hi, I have ulcerative colitis but been I have been in remission for quite some time now(2-3 months). My hair doesn’t seem to be growing back although I am still hoping for the results found in this article, any advice?Oh and thank you for posting this!
I needed to read this article. The last time I experienced this drastic amount of hair loss ( 12 years ago) I was malnourished from mal-absorption for over a year. Still no diagnoses on the gut issues I had been experiencing since I was 10 years old ( I am now 60). I was admitted to hospital for 13 1/2 months and on TPN. About a year ago I noticed hair loss and asked my doctor if I could go on a B12 supplement. I was denied not just once but four times. I realized that I too had a part in the NO answer. I had failed to tell him that I was experiencing a ton of hair loss ( not to mention many other symptoms and, he too had failed to ask me why I thought I needed B12. I learned something there big time. This article has set me at ease. I have been on B12 shots for three months now and still no little bristles growing back yet. I am however dealing with mal-absorption again tho I was aware of something happening a year ago, I had no idea at the time it was my now diagnosed UC. Thank you so much for such amazing information. The last name “Sharp” has played an important role in my diagnoses. A Dr. Russel Sharp in Vancouver…any relation?
Hi Linda,
I apologize for the late response. I really appreciate your comment. I’m sorry to hear about all of the issues you’ve faced; I hope things are improving for you now. I don’t believe I’m related to Dr. Russel Sharp, but I’m glad to hear he’s putting our namesake to good use :-). Take care!
I have had C Dif now for over 5 months in which I have been prescribed Flagyl once, Vancomyacin three times and have just finished Dificid as the last prescribed drug which seems to of cured this horrible symdrome. I, however, have always had beautiful full thick hair which is now thin and limp and matting and falling out at an alarming rate. Could this be from having had C Dif for over 5 months? I am trying to find out if there has been any research on this as one of the side effects of this horrendous pest.
Thank you for this excellent article. It helped me a lot in the months after my diagnosis with UC when alarming amounts of my hair started to fall out (it all grew back fine).
I see people asking about hair loss in online support groups for IBD, and it’s clear that hair loss is very distressing on top of a diagnosis of a chronic illness, and all that that entails.
Because of your article, I asked Crohn’s & Colitis UK to include information about Telogen Effluvium in their literature for IBD patients, and I’m pleased that they now have.